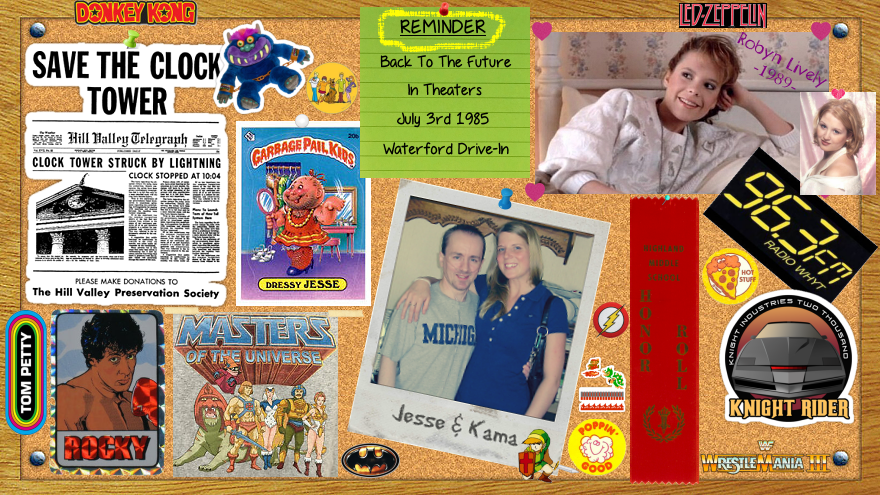
by Jesse Richardson
Inspired by someone I once knew:
Locals knew her as Hilltop girl, I knew her as a friend.
Quiet, sweet, shy, and strong.
So many things I wanted to tell her, too afraid.
I missed her since her departure to the hills, never to be seen again.
I strolled along the road hoping to see her behind her window.
Her blonde hair soft as cotton, precious as gold, free as a butterfly.
Memories of a weekend I won't forget, memories fallen away.
A smile so bright, to shine a city.
Kindness that warms a room with happiness.
I stopped to glance at the hilltop, a fortress of wonder.
Loneliness we shared, she never knew.
Loneliness we shared, she never knew.
Wonder if she was ever told that she was special?
A piece of her was lost, lost into the clouds to never return.
A sister to never be seen, heard, or spoken to again.
A friend she needed.
Surrounded by trees, surrounded by an illness.
As I looked at her home, I wondered about her.
Wish I could have told her things were going to be fine, I'm here.
Wish I could have stepped back a bit, let her come to me.
Being too nice is a downfall.
Being too nice is a downfall.
Looking at the hilltop, she wasn't coming to me.
Teardrop of salt hit the ground.
Just a wish I had wished for.
Just a wish I had wished for.
To see her again, to make things right, to make them better.
Niceness can be a deadly weapon, to make others drift away.
Drift away as Hilltop girl has done.
As I walked around, mist from the clouds spoke.
I could hear her voice without being spoken to.
Never to be seen, never spoken to.
I wished. . . one last time.
I wished. . . one last time.
To hug her, to say hi, to never say goodbye.
To do it all over again, I would change a few things.
Birds flew past her window as if to signal I was there.
A smile I saw through the window.
A gleam, a glow, a face.
A precious face I saw.
A smile I saw through the window.
A gleam, a glow, a face.
A precious face I saw.
With a tear drop on my pillow, I woke up.
A dream.
A dream.
That was all.
A hope.
That was all.
To see her again, a dream I had hoped for.
A hope.
That was all.
To see her again, a dream I had hoped for.
She was somebody that I us to know.